Abstract
Background: The pandemic of COVID-19 (Coronavirus disease 2019) impacted the practices of blood product procurement and transfusion in multiple ways, including failed blood donation drives, staffing limitations and low donor turnout. On January 1, 2022, the American Red Cross declared the worst national blood crisis in over a decade. The effect was most notable on the community medical centers with limited resources in securing products for blood transfusion. However, evidence is lacking for the usage of blood products in a community teaching hospital during this pandemic.
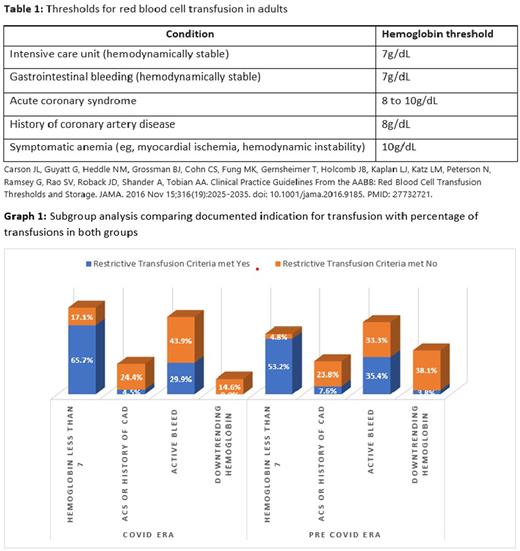
Study Design and Methods: We aimed to contrast the adherence to restrictive transfusion practice in the COVID era with the pre-COVID era irrespective of COVID-19 diagnosis. We performed a retrospective observational study involving packed red blood cell (PRBC) transfusions in patients from June 2020 to August 2020 (COVID era) and September 2019 to November 2019 (pre-COVID era). Patients with hemoglobinopathies were excluded. A detailed chart review to include the number of PRBC transfusions, documented indication for transfusion and it was also determined if transfusions met restrictive blood transfusion criteria (as per guidelines from the Association for the Advancement of Blood & Biotherapies (AABB)) (Table 1). Demographic data included age, gender, history of coronary artery disease (CAD) or prior gastrointestinal bleed, use of antiplatelet and anticoagulation, use of deep vein thrombosis prophylaxis inpatient, and diagnosis on admission. Chi-square was applied to test the statistical association between qualitative variables and Unpaired t-test/Mann Whitney U test was applied to test the mean difference of quantitative. The level of significance was set at 5%.
Results: A total of 215 patients were screened and 208 met our inclusion criteria. There were 108 PRBC transfusions in the COVID era group and 100 PRBC transfusions in the pre-COVID era group, with equal distribution in both groups for age, sex, ethnicity and prior gastrointestinal bleed. The leading diagnosis on admission in both COVID era and pre-COVID era groups was acute hypoxia (53.7% and 36% p<0.001), followed by gastrointestinal bleeding. Lower proportion of patients receiving transfusion were on anticoagulant or antiplatelet therapy in COVID era group as compared to pre-COVID era (antiplatelet: 6.2% vs 19%, p<0.001 and anticoagulant: 12.1% vs 27%, p<0.001), though COVID era group had lower fraction of patients receiving pharmacological prophylaxis for deep vein thrombosis (DVT) (13.9% vs 29%, p<0.001). There was a higher percentage of transfusions in critical care units in the COVID era group than pre-COVID era group (38.9% vs 22%, p<0.008). Documented indications for transfusions in both groups were hemoglobin < 7 (47.2% vs 43%), acute coronary syndrome (ACS) or history of CAD (12% vs 11%), active bleed (35.2% vs 35%) and down trending hemoglobin (5.6% vs 11%).
Restrictive transfusion criteria were met in only 67% vs 79% in COVID era and pre-COVID era transfusion cases respectively (p=0.008). Subgroup analysis of documented indications for transfusion among both groups is displayed in Graph 1.
Conclusions: As evident from our results, the COVID era group despite having comparable, if not fewer risk factors associated with blood loss, received blood transfusion with less stringent adherence to restrictive blood transfusion guidelines. COVID pandemic had a significant impact on the landscape of blood transfusion and our study brought to light the physician's role in more liberal use of blood products. Due to a higher number of critical care admissions and the morbidity/mortality during this pandemic, compel physicians to have a more liberal mindset towards blood transfusions. However, given the acute shortage of blood products it is vital that we adhere to restrictive blood transfusion guidelines.
In view of the ongoing National Blood Crisis, please visit RedCrossBlood.org or call 1-800-RED CROSS (1-800-733-2767) to donate blood.
Disclosures
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal